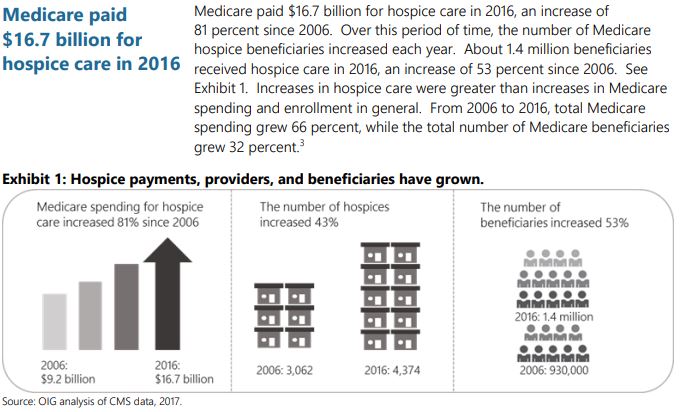
 A report released recently released by the Office of Inspector General (OIG) at the US Department of Health titled: Vulnerabilities in the Medicare Hospice Program Affect Quality Care and Program Integrity has highlighted that hospice care fraud is a nationwide problem in the US. The report found that hospices do not always provide needed services to beneficiaries and sometimes provide poor quality care for Nursing home residents and other patients. When care is provided hospices’ inappropriate billing costs Medicare hundreds of millions of dollars (n 2016, Medicare paid hospice providers $16.7 billion. A decade earlier, it was $9.2 billion, according to reports). Several schemes of fraud in nursing facilities identified in the report included but is not limited to:
A report released recently released by the Office of Inspector General (OIG) at the US Department of Health titled: Vulnerabilities in the Medicare Hospice Program Affect Quality Care and Program Integrity has highlighted that hospice care fraud is a nationwide problem in the US. The report found that hospices do not always provide needed services to beneficiaries and sometimes provide poor quality care for Nursing home residents and other patients. When care is provided hospices’ inappropriate billing costs Medicare hundreds of millions of dollars (n 2016, Medicare paid hospice providers $16.7 billion. A decade earlier, it was $9.2 billion, according to reports). Several schemes of fraud in nursing facilities identified in the report included but is not limited to:
- Billing and overcharging for an expensive level of care that is unnecessary
- Hospice providers would seek out patients who live in nursing homes or assisted living
- Enrolling beneficiaries who are not eligible for hospice care
- Physicians received payment for recruiting patients who were not terminally ill to hospice centers
- Billing and overcharging for services never provided
- Patient referral kickbacks and falsifying documentation
- Providing fewer services than outlined in care plans
- Providers neglect to share crucial information to help nursing home residents make informed decisions.
OIG evaluations and audits have raised concerns about hospice billing, Federal oversight, and quality of care provided to beneficiaries. The OIG’s 45-page report addressed several actions to strengthen the hospice program including strengthening the survey process to better ensure that hospices provide beneficiaries with quality care and necessary services; giving the federal government more authority to address poor-performing hospice providers; educating nursing home residents and their families about the hospice benefit; and strengthening oversight of hospice providers to reduce inappropriate billing, according to news sources.
